jesoga70therapy medical mission/light of divine shadows
0919606 0022 /226 27 24
www.jesoga70therapymedicalmission.webs.com

Coronary artery bypass surgery, also coronary artery bypass graft (CABG pronounced cabbage) surgery, and colloquially heart bypass or bypass surgery is a surgical procedure performed to relieve angina and reduce the risk of death from coronary artery disease. Arteries or veins from elsewhere in the patient's body are grafted to the coronary arteries to bypass atherosclerotic narrowings and improve the blood supply to the coronary circulation supplying the myocardium (heart muscle). This surgery is usually performed with the heart stopped, necessitating the usage of cardiopulmonary bypass; techniques are available to perform CABG on a beating heart, so-called "off-pump" surgery.
History
The first coronary artery bypass surgery was performed in the United States on May 2, 1960, at the Albert Einstein College of Medicine-Bronx Municipal Hospital Center by a team led by Dr. Robert Goetz and the thoracic surgeon, Dr. Michael Rohman with the assistance of Dr. Jordan Haller and Dr. Ronald Dee.[1][2] In this technique the vessels are held together with circumferential ligatures over an inserted metal ring. The internal mammary artery was used as the donor vessel and was anastomosed to the right coronary artery. The actual anastomosis with the Rosenbach ring took fifteen seconds and did not require Cardio-Pulmonary bypass. The disadvantage of using the internal mammary artery was that, at autopsy nine months later, the anastomosis was open, but an atheromatous plaque had occluded the origin of the internal mammary that was used for the bypass.[citation needed][verification needed]
Russian cardiac surgeon, Dr. Vasilii Kolesov, performed arguably the first successful internal mammary artery–coronary artery anastomosis in 1964.[3][4]
However, Goetz's has been cited by others, including Kolesov,[5] as the first successful human coronary artery bypass.[6][7][8][9][10][11][12] Goetz's case has frequently been overlooked. Confusion has persisted for over 40 years and seems to be due to the absence of a full report and to misunderstanding about the type of anastomosis that was created. The anastomosis was intima-to-intima, with the vessels held together with circumferential ligatures over a specially designed metal ring. Kolesov did the first successful coronary bypass using a standard suture technique in 1964, and over the next five years he performed 33 sutured and mechanically stapled anastomoses in St. Petersburg, Russia.[13][14]
Dr. René Favaloro, an Argentine surgeon, achieved a physiologic approach in the surgical management of coronary artery disease—the bypass grafting procedure—at the Cleveland Clinic in May 1967.[4][15] His new technique used a saphenous vein autograft to replace a stenotic segment of the right coronary artery. Later, he successfully used the saphenous vein as a bypassing channel, which has become the typical bypass graft technique we know today; in the U.S., this vessel is typically harvested endoscopically, using a technique known as endoscopic vessel harvesting (EVH). Soon Dr. Dudley Johnson extended the bypass to include left coronary arterial systems.[4] In 1968, Doctors Charles Bailey, Teruo Hirose and George Green used the internal mammary artery instead of the saphenous vein for the grafting.[4]
Arteriosclerosis is a common arterial disorder characterized by thickening, loss of elasticity, and calcification of arterial walls, resulting in a decreased blood supply.
Atherosclerosis is a common arterial disorder characterized by yellowish plaques of cholesterol, lipids, and cellular debris in the inner layer of the walls of large and medium-sized arteries.
A greater number of bypasses does not imply a person is "more sick", nor does a lesser number imply a person is "healthier."[17] A person with a large amount of coronary artery disease (CAD) may receive fewer bypass grafts owing to the lack of suitable "target" vessels. A coronary artery may be unsuitable for bypass grafting if it is small (< 1 mm or < 1.5 mm depending on surgeon preference), heavily calcified (meaning the artery does not have a section free of CAD) or intramyocardial (the coronary artery is located within the heart muscle rather than on the surface of the heart). Similarly, a person with a single stenosis ("narrowing") of the left main coronary artery requires only two bypasses (to the LAD and the LCX). However, a left main lesion places a person at the highest risk for death from a cardiac cause.[citation needed]
The surgeon reviews the coronary angiogram prior to surgery and identifies the lesions (or "blockages") in the coronary arteries. The surgeon will estimate the number of bypass grafts prior to surgery, but the final decision is made in the operating room upon examination of the heart.
The Surgery or Stent (SoS) trial was a randomized controlled trial that compared CABG to PCI with bare-metal stents. The SoS trial demonstrated CABG is superior to PCI in multivessel coronary disease.[19]
The SYNTAX trial was a randomized controlled trial of 1800 patients with multivessel coronary disease, comparing CABG versus PCI using drug-eluting stents (DES). The study found that rates of major adverse cardiac or cerebrovascular events at 12 months were significantly higher in the DES group (17.8% versus 12.4% for CABG; P=0.002).[20] This was primarily driven by higher need for repeat revascularization procedures in the PCI group with no difference in repeat infarctions or survival. Higher rates of strokes were seen in the CABG group.
The FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus—Optimal Management of Multivessel Disease) trial will compare CABG and DES in patients with diabetes. The registries of the nonrandomized patients screened for these trials may provide as much robust data regarding revascularization outcomes as the randomized analysis.[21]
A study comparing the outcomes of all patients in New York state treated with CABG or percutaneous coronary intervention (PCI) demonstrated CABG was superior to PCI with DES in multivessel (more than one diseased artery) coronary artery disease (CAD). Patients treated with CABG had lower rates of death and of death or myocardial infarction than treatment with a coronary stent. Patients undergoing CABG also had lower rates of repeat revascularization.[22] The New York State registry included all patients undergoing revascularization for coronary artery disease, but was not a randomized trial, and so may have reflected other factors besides the method of coronary revascularization.
The 2004 ACC/AHA CABG guidelines state CABG is the preferred treatment for:[23]
0919606 0022 /226 27 24
www.jesoga70therapymedicalmission.webs.com
Coronary artery bypass surgery
how jesoga70therapy works to bypass/stroke patient
01. mr. juan d la cruz / bypass victim recovered by energizing the heart. by touching the 14 vitality abdominal impluses functioning system. residing at 300 sto rosario st., mandaluyong city . construction of blood circulation into the ventricles relax heartbeat cycles stay normal . in one single touch jesoga therapy proven speed healing done., the therapy still going on the patient seem's batista brother (bodysized)
2) Ms juan D la Cruz 76 yrs of age from Zamboanga city , temporary residing at mb 27 rm112 suffer from heart problem and schedule 4 bypass operation at V. luna hospital at Quezon city that day when the family notify us because the operation was being cancelled due to hypertension. 9pm that night the family called us because the patient had shortness of breathings and they confirm it's to late to rush the patient to the hospitals. The situation really serious the patient is not talking anymore but the jesoga70therapy technique was trained mostly at these kind of retrival life saving condition. It's really a meracles for the family after touching there 14 vitality abdominal impulses the patient went up and find the restroom (for bowel ) and speak to them , she's wandering how the touch's energize the heart muscle and stimulate the normal blood circulation take away the accumulation cholesterol in the blood stream, stop bleeding and promote the healing just a matter of 10 seconds. My dear view the family came from the marine, and phil nationa police forces ., these is the true story how jesoga70therapy is working to the human body(fatal) ? even the neighborhood exactly witness these testimony , we really want to secure every little pieces of our reliable information to the best of our ability to served the poor people from their badhealth and financially sufferings/loss. So anyone from you , is welcome to investigate these case whatever entention theroff.(kuya neck) who own the unit. PnP personnel from camp crame Quezon city.
From.
| This article needs additional citations for verification. Please help improve this article by adding reliable references. Unsourced material may be challenged and removed. (March 2008) |
| Coronary artery bypass surgery | |
|---|---|
| Intervention | |
 Early in a coronary artery bypass surgery during vein harvesting from the legs (left of image) and the establishment of bypass (placement of the aortic cannula) (bottom of image). The perfusionist and heart-lung machine (HLM) are on the upper right. The patient's head (not seen) is at the bottom. | |
| ICD-10-PCS | 021209W |
| ICD-9-CM | 36.1 |
| MeSH | D001026 |
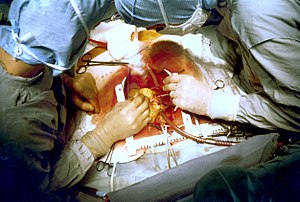
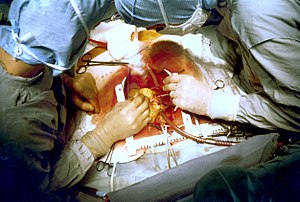
Coronary artery bypass surgery during mobilization (freeing) of the right coronary artery from its surrounding tissue, adipose tissue (yellow). The tube visible at the bottom is the aortic cannula (returns blood from the HLM). The tube above it (obscured by the surgeon on the right) is the venous cannula (receives blood from the body). The patient's heart is stopped and the aorta is cross-clamped. The patient's head (not seen) is at the bottom.

Three coronary artery bypass grafts, a LIMA to LAD and two saphenous vein grafts - one to the right coronary artery (RCA) system and one to the obtuse marginal (OM) system.
History
The first coronary artery bypass surgery was performed in the United States on May 2, 1960, at the Albert Einstein College of Medicine-Bronx Municipal Hospital Center by a team led by Dr. Robert Goetz and the thoracic surgeon, Dr. Michael Rohman with the assistance of Dr. Jordan Haller and Dr. Ronald Dee.[1][2] In this technique the vessels are held together with circumferential ligatures over an inserted metal ring. The internal mammary artery was used as the donor vessel and was anastomosed to the right coronary artery. The actual anastomosis with the Rosenbach ring took fifteen seconds and did not require Cardio-Pulmonary bypass. The disadvantage of using the internal mammary artery was that, at autopsy nine months later, the anastomosis was open, but an atheromatous plaque had occluded the origin of the internal mammary that was used for the bypass.[citation needed][verification needed]
Russian cardiac surgeon, Dr. Vasilii Kolesov, performed arguably the first successful internal mammary artery–coronary artery anastomosis in 1964.[3][4]
However, Goetz's has been cited by others, including Kolesov,[5] as the first successful human coronary artery bypass.[6][7][8][9][10][11][12] Goetz's case has frequently been overlooked. Confusion has persisted for over 40 years and seems to be due to the absence of a full report and to misunderstanding about the type of anastomosis that was created. The anastomosis was intima-to-intima, with the vessels held together with circumferential ligatures over a specially designed metal ring. Kolesov did the first successful coronary bypass using a standard suture technique in 1964, and over the next five years he performed 33 sutured and mechanically stapled anastomoses in St. Petersburg, Russia.[13][14]
Dr. René Favaloro, an Argentine surgeon, achieved a physiologic approach in the surgical management of coronary artery disease—the bypass grafting procedure—at the Cleveland Clinic in May 1967.[4][15] His new technique used a saphenous vein autograft to replace a stenotic segment of the right coronary artery. Later, he successfully used the saphenous vein as a bypassing channel, which has become the typical bypass graft technique we know today; in the U.S., this vessel is typically harvested endoscopically, using a technique known as endoscopic vessel harvesting (EVH). Soon Dr. Dudley Johnson extended the bypass to include left coronary arterial systems.[4] In 1968, Doctors Charles Bailey, Teruo Hirose and George Green used the internal mammary artery instead of the saphenous vein for the grafting.[4]
Terminology
There are many variations on terminology, in which one or more of "artery", "bypass" or "graft" is left out. The most frequently used acronym for this type of surgery is CABG (pronounced 'cabbage'),[16] pluralized as CABGs (pronounced 'cabbages'). More recently[when?] the term aortocoronary bypass (ACB) has come into popular use. CAGS (Coronary Artery Graft Surgery, pronounced phonetically) should not be confused with Coronary Angiography (CAG).Arteriosclerosis is a common arterial disorder characterized by thickening, loss of elasticity, and calcification of arterial walls, resulting in a decreased blood supply.
Atherosclerosis is a common arterial disorder characterized by yellowish plaques of cholesterol, lipids, and cellular debris in the inner layer of the walls of large and medium-sized arteries.
Number of bypasses
The terms single bypass, double bypass, triple bypass, quadruple bypass and quintuple bypass refer to the number of coronary arteries bypassed in the procedure. In other words, a double bypass means two coronary arteries are bypassed (e.g. the left anterior descending (LAD) coronary artery and right coronary artery (RCA)); a triple bypass means three vessels are bypassed (e.g. LAD, RCA, left circumflex artery (LCX)); a quadruple bypass means four vessels are bypassed (e.g. LAD, RCA, LCX, first diagonal artery of the LAD) while quintuple means five. Bypass of more than four coronary arteries is uncommon.A greater number of bypasses does not imply a person is "more sick", nor does a lesser number imply a person is "healthier."[17] A person with a large amount of coronary artery disease (CAD) may receive fewer bypass grafts owing to the lack of suitable "target" vessels. A coronary artery may be unsuitable for bypass grafting if it is small (< 1 mm or < 1.5 mm depending on surgeon preference), heavily calcified (meaning the artery does not have a section free of CAD) or intramyocardial (the coronary artery is located within the heart muscle rather than on the surface of the heart). Similarly, a person with a single stenosis ("narrowing") of the left main coronary artery requires only two bypasses (to the LAD and the LCX). However, a left main lesion places a person at the highest risk for death from a cardiac cause.[citation needed]
The surgeon reviews the coronary angiogram prior to surgery and identifies the lesions (or "blockages") in the coronary arteries. The surgeon will estimate the number of bypass grafts prior to surgery, but the final decision is made in the operating room upon examination of the heart.
Indications for CABG
Several alternative treatments for coronary artery disease exist. They include:- Medical management (anti-anginal medications plus statins, antihypertensives, smoking cessation, tight blood sugar control in diabetics)
- Percutaneous coronary intervention (PCI)
The Surgery or Stent (SoS) trial was a randomized controlled trial that compared CABG to PCI with bare-metal stents. The SoS trial demonstrated CABG is superior to PCI in multivessel coronary disease.[19]
The SYNTAX trial was a randomized controlled trial of 1800 patients with multivessel coronary disease, comparing CABG versus PCI using drug-eluting stents (DES). The study found that rates of major adverse cardiac or cerebrovascular events at 12 months were significantly higher in the DES group (17.8% versus 12.4% for CABG; P=0.002).[20] This was primarily driven by higher need for repeat revascularization procedures in the PCI group with no difference in repeat infarctions or survival. Higher rates of strokes were seen in the CABG group.
The FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus—Optimal Management of Multivessel Disease) trial will compare CABG and DES in patients with diabetes. The registries of the nonrandomized patients screened for these trials may provide as much robust data regarding revascularization outcomes as the randomized analysis.[21]
A study comparing the outcomes of all patients in New York state treated with CABG or percutaneous coronary intervention (PCI) demonstrated CABG was superior to PCI with DES in multivessel (more than one diseased artery) coronary artery disease (CAD). Patients treated with CABG had lower rates of death and of death or myocardial infarction than treatment with a coronary stent. Patients undergoing CABG also had lower rates of repeat revascularization.[22] The New York State registry included all patients undergoing revascularization for coronary artery disease, but was not a randomized trial, and so may have reflected other factors besides the method of coronary revascularization.
The 2004 ACC/AHA CABG guidelines state CABG is the preferred treatment for:[23]
- Disease of the left main coronary artery (LMCA).
- Disease of all three coronary vessels (LAD, LCX and RCA).
- Diffuse disease not amenable to treatment with a PCI.

Walang komento:
Mag-post ng isang Komento